Understanding the Alzheimer Clock is increasingly recognized as a pivotal factor in enhancing early detection strategies for Alzheimer's disease. As the global health community faces the burgeoning challenge of dementia, reports indicate that nearly 50 million people worldwide are living with Alzheimer's, a number expected to rise to 152 million by 2050 (World Health Organization, 2021). The Alzheimer Clock, which refers to a novel framework for identifying the disease's progression timeline, offers a transformative approach toward early diagnosis, intervention, and ultimately, patient care.
Dr. Sarah Thompson, a leading neurologist specializing in Alzheimer's research, emphasizes the significance of the Alzheimer Clock, stating, "By understanding the timing of biological changes associated with Alzheimer's, we can leverage early warning signals that may lead to timely interventions." This paradigm shift in perception underscores the necessity for healthcare professionals to adopt this innovative model in their diagnostic practices. Early detection not only benefits patients and their families but also has profound implications for healthcare resources and overall societal impact, making the Alzheimer Clock an essential element of contemporary Alzheimer's research and treatment strategies.

The concept of the Alzheimer Clock represents a groundbreaking approach in neurodegenerative research, aiming to track the complex progression of Alzheimer's disease through temporal markers. Researchers have identified that neurodegenerative changes follow a predictable trajectory over time, often beginning years or even decades before clinical symptoms manifest. According to a study published in the journal *Nature Aging*, by the time individuals reach the early stages of cognitive decline, significant pathological changes related to Alzheimer's, such as amyloid plaque accumulation, could already be underway, suggesting a temporal 'clock' that ticks down to cognitive impairment.
Recent advancements in neuroimaging and biomarker analysis have led scientists to refine this clock model, providing a timeline for diagnosing and understanding Alzheimer's pathology. The Alzheimer's Association's 2023 report highlights that early detection strategies enhanced by the Alzheimer Clock concept could potentially improve patient outcomes, as it could allow for interventions during the asymptomatic phase. As of now, it is estimated that over 6 million Americans are living with Alzheimer’s, and this number is projected to increase significantly. By harnessing the power of the Alzheimer Clock, healthcare professionals can develop personalized strategies for monitoring and addressing the disease, paving the way for a future where early diagnosis becomes the norm rather than the exception.
This bar chart illustrates the estimated years for progression through different stages of Alzheimer’s disease. Understanding these stages is crucial for developing effective early detection strategies and interventions.
Understanding the progression of Alzheimer's disease through the concept of the "Alzheimer Clock" is pivotal in advancing early detection strategies. This theoretical framework emphasizes crucial biomarkers that indicate the disease's development over time, offering a pathway for interventions before significant cognitive decline occurs. Research indicates that specific changes in biomarkers such as amyloid-beta and tau proteins can be detected years, if not decades, before clinical symptoms emerge. According to a report from the Alzheimer's Association, the presence of these biomarkers can provide insights about individual risk profiles and guide personalized monitoring approaches.
Furthermore, emerging studies highlight the importance of neuroinflammation and neurodegeneration markers as integral components of the Alzheimer Clock. The use of advanced imaging technologies and genetic analysis allows for a more precise understanding of the pathological processes at play. For instance, a study published in the journal *Nature Reviews Neurology* suggests that measuring levels of neurofilament light chain (NfL) in the blood can serve as an effective indicator of neurodegeneration linked to Alzheimer's progression. By focusing on these key biomarkers, healthcare providers can implement more robust early detection strategies, enabling timely therapeutic interventions and potentially altering the disease trajectory for individuals at risk.
| Biomarker | Role in Alzheimer’s | Stage of Progression | Detection Method | Clinical Relevance |
|---|---|---|---|---|
| Amyloid Beta | Formation of plaques disrupting cell communication | Early | PET Imaging, CSF Analysis | High predictive value for Alzheimer's diagnosis |
| Tau Protein | Forms tangles within neurons leading to cell death | Moderate | CSF Analysis, PET Imaging | Indicates neurodegeneration severity |
| Neurogranin | Marker of synaptic integrity | Preclinical | Blood Test | Emerging biomarker for early detection |
| YKL-40 | Involved in inflammation and neurodegeneration | Mild Cognitive Impairment | Blood Test | Related to cognitive decline |
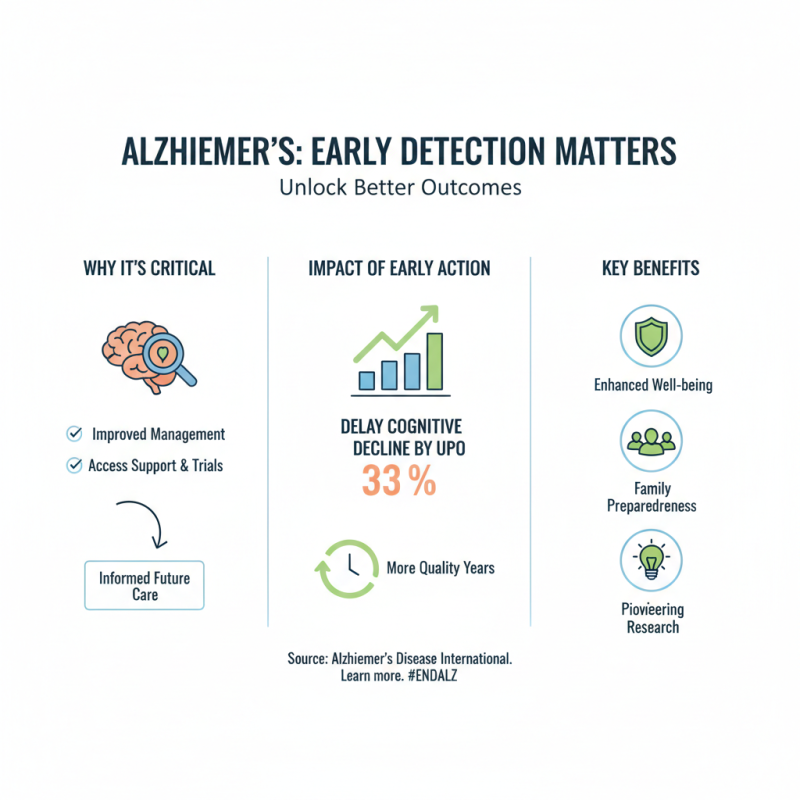
Early detection of Alzheimer's disease is a critical factor that significantly influences the management and progression of the illness. According to a report from Alzheimer's Disease International, timely diagnosis can lead to improved outcomes, allowing patients and families to access essential support services, participate in clinical trials, and make informed decisions about future care. Studies indicate that early intervention may delay cognitive decline by up to 33%, emphasizing the necessity of recognizing the signs of the disease as early as possible.
Implementing proactive assessment strategies can also enhance the effectiveness of current treatment options. Individuals showing early signs, such as mild cognitive impairment, have a better chance of benefiting from available therapies. For instance, the Alzheimer's Association has highlighted that patients who engage in cognitive stimulation and lifestyle modifications within the early stages experience a slower progression of symptoms. Therefore, educating the community about the "Alzheimer Clock" can cultivate an awareness that leads to earlier consultations and diagnostics.
Tips: Encourage regular cognitive screenings, especially for those with a family history of Alzheimer’s. Engaging in lifestyle changes—like exercise, diet, and mental challenges—can promote brain health and potentially delay the onset of symptoms. Keeping track of cognitive changes can empower individuals to seek medical advice when necessary.
Innovative technologies are transforming the approach to monitoring the Alzheimer Clock, a concept that refers to the time-sensitive biomarkers indicating the onset of Alzheimer’s disease. Early detection is crucial, as it can significantly alter the course of care and management for individuals at risk. In recent years, advancements in neuroimaging techniques, artificial intelligence, and wearable health devices have emerged as powerful tools in tracking these essential biomarkers. These innovations not only provide real-time data but also enhance the accuracy of predictions regarding cognitive decline.
To optimize the use of these technologies for Alzheimer detection, consider implementing some practical tips. Regular cognitive assessments through mobile applications can help capture subtle changes in memory and thinking skills over time. Additionally, engaging with wearable devices that monitor physical and mental activities may offer insights into changes that precede clinical symptoms, allowing for earlier intervention. It’s also vital to maintain open communication with healthcare providers, ensuring that any changes in health status are properly monitored and addressed.
The integration of these innovative technologies into healthcare practices marks a significant shift towards proactive management of cognitive health. By utilizing these tools and adopting a preventive mindset, individuals and healthcare systems can work collaboratively to transform outcomes for those at risk of developing Alzheimer’s disease.
Recent advancements in Alzheimer clock research are paving the way for transformative early detection strategies that may significantly alter the landscape of Alzheimer’s disease management. The Alzheimer clock, a biological marker linked to the disease's progression, quantifies the biological age of an individual relative to their chronological age, providing critical insights into cognitive decline risk. According to a report by the Alzheimer's Association, approximately 6.5 million Americans are currently living with Alzheimer's, and early diagnosis remains a cornerstone of effective intervention, potentially delaying the onset of severe symptoms.
Future directions in Alzheimer clock research suggest a multi-faceted approach combining genetic, biomarker, and lifestyle data to enhance detection strategies. Studies indicate that integrating cognitive assessments and neuroimaging with genetic predisposition data could elevate predictive accuracy. For instance, a study published in the Journal of Alzheimer's Disease highlighted that utilizing machine learning techniques on data from thousands of participants led to a 20% increase in the accuracy of predicting Alzheimer’s onset compared to conventional methods. This shows a promising trajectory for personalized early interventions, enabling healthcare providers to tailor preventive measures based on an individual's Alzheimer clock metrics.